1. They’re on a Bad Streak
Nurses are skilled professionals. They spend time perfecting their art of nursing, which includes IV sticks, lab draws, catheter insertions, central line care, wound packing and dressings, and the list goes on.
However, nurses are human. We have good and bad days, streaks of perfection and, well, streaks of failure. There are nurses who seem to possess superpowers, those who seem close to godliness in the skillful way they find veins in the most edematous of patients and place a Foley catheter in the darkest and most confusing recesses of the human body. These are the rarest of nurses, and they make the rest of us feel quite inept.
So, if you ask a nurse, “how good are you at this?” or “how many times have you done this before?” the answers may vary, but we will always sound confident because pessimism does not work well in our occupation. If we’re on a bad streak (specifically with IV insertion), we’re hoping you’ll be the lucky star who turns it around and sends us back to our streak of perfection.
Keep in mind that you can always request another nurse, someone more specialized, or a pediatric nurse (as they seem to hold the IV-insertion superpower). But whatever you do, please don’t doubt our motive: We strive to be perfect at what we do, every time.
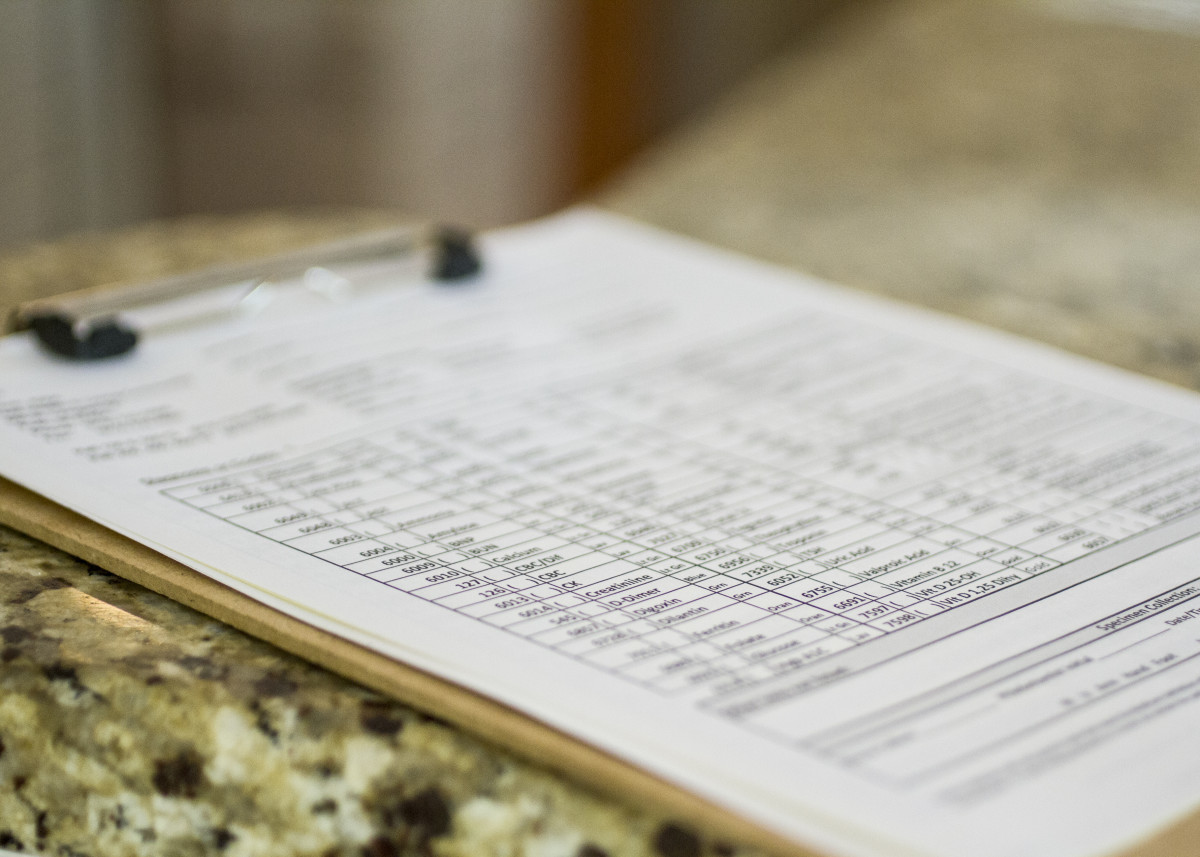
2. They Know Preliminary Test Results
Yes, that’s right, we know the answer to your diagnostic test, but we’re not always the right person to tell you. It has to do with hospital policy and politics. We often know results first, since nurses act as the messenger between pathologists, radiologists, and primary providers. Some nurses leave the results for the patient’s healthcare provider (physician, PA, or NP) to deliver, while others use their own judgment to decide what they can safely share with their patients without digging a hole they can’t get out of.
Your best bet? Wait for your healthcare provider to ask the important questions. It’s hard to wait, but you can use that time to make a list of all the things you’d like to ask. That way, your mind won’t come up blank when they finally show up, and you’ll save your nurse a moral dilemma.

3. The Patient Next Door Is Dying
Nurses always seem busy, rushed, and quick to move on to the next patient, barely leaving time to make conversation or inquire more about how you’re feeling today. That is because we are busy, extremely busy trying to stay focused, avoid mistakes, and above all, keep our patients safe. We’re busy trying to keep confused patients in their chairs, hurting patients pain-free, post-op patients walking, coughing, and breathing, and dying patients comfortable.
Of all these people, the dying patients and their families require the most care, comfort, compassion, and attention. On a good day, nurses are typically given a lighter load when providing care to those destined for their celestial transfer, but even then it’s difficult to equally distribute attention to every patient. Most people don’t come to the hospital to die, nor do they want to know if someone is dying, especially if it’s their “neighbor.” We’re good at keeping secrets: Even if it wasn’t mandated by federal law, we always strive to keep a straight face and focus entirely on the patient at hand. But it’s hard to deny it when patients notice the somber faces of fellow visitors and the sound of tears next door.
So if you’re ever in this position, please give your nurses a little extra patience that day, because compassionate care is a difficult job and a little kindness goes a long way.

4. They Had to Google It
So, you’re admitted with a unique and rare disease. It may be a condition that your nurses are not familiar with. Whenever we don’t understand a disease or know the answer to your question, you can be sure that we are actively searching for the answer online. Let’s just hope that your nurse uses a legitimate medical evidence-based resource such as UpToDate rather than Wikipedia.
Additionally, if you or your family member want to look up information, become an amateur diagnostician, or maybe just read more about your condition, please use legitimate medical websites and not Wikipedia or someone’s terrifying blog account. It’s nice to know things, but inadequate, biased, or fallacious websites can be a dangerous thing.

5. They Don’t Remember Your Name
Due to the Health Insurance Portability & Accountability Act (Title II), we keep patient information top-secret. To prevent revealing information to other patients and visitors in the hallways and shared rooms, you may overhear us calling you by your room number.
Many times it will be, “Will you please get 3B some ice,” or “6C would like to shower now” to our fellow aides, but it’s not that we don’t care enough to remember your names. We truly do, especially if we have the joy of keeping you for our 3-day/36-hour stretch of the week. (This isn’t sarcastic: We are genuinely excited if we can provide continuity of care and help you improve, especially if we can exchange end-of-shift reports with the same nurse). Sometimes, though, it’s just easier and more efficient to call you by your room name.
But truth be told, there may be moments when your name eludes us. Believe me, I’m excellent at remembering names and even better at faces, but barely two hours into a morning shift, downing hospital-brewed Sanka that pretends to be coffee, and remembering I have six patients to assess, look up labs for, prep for tests, and give meds to by 10 a.m., my mind may come up with a blank when your family member calls, wondering how you’re doing that morning. Don’t worry though, I’ll have your name down by 7 p.m…. unless of course I’ve overused your name that day, and that’s not always a good thing.

6. Being “Discharged” Does NOT Mean You Can Go Home Now
Okay, so this is something we probably want you to know.
When a physician tells you that you’re going home in the morning, it doesn’t always mean before 11 a.m. In the hospital world, there are a lot of “ifs” and “buts” to determine exactly when you will be discharged.
First: Why are you here? If you’re in the hospital for any exacerbation of a chronic disease (heart failure, COPD, or uncontrolled diabetes, for example), you most likely require education before being sent home. New medications such as Coumadin or Lovenox also require extra education. Don’t be surprised if this delays your discharge.
Second: Who said you could go home? Was it your specialist? If so, this simply means that they’ve discharged you from their standpoint. The rest of the process of discharge then falls to the remaining specialists, and if none remain, it is left for the primary provider (typically a Hospitalist or Internal Medicine group). If you are admitted solely under a specialist (for example, you’re admitted under an orthopedic surgeon for a knee replacement), then it’s safe to say you are truly discharged.
Third: “My doc says I’m discharged, so I’ll go ahead and take my IV out in order to save my nurse some time, right?” The answer is NO! Please ask your nurse first and please don’t take it out yourself. There are many things that can delay a discharge: laboratory tests, required repeat labs that were lost in the tube system or had erroneous results, a surprise fever, a case of syncope (passing out), or (god forbid) a serious event such as a heart arrhythmia or cardiac/respiratory arrest. These are some of the reasons why you should not take out that IV; your nurse will thank you.
Fourth: Above all, be patient. If you’ve asked your nurse when you will be discharged more than four times in a single hour, you’ve most likely delayed your discharge even further. Every trek back into a patient’s room to reassure them that they will be discharged “soon” takes time away from passing out meds, toileting patients, and sending them for tests so that the nurse can finally sit down and write out your discharge papers. If you’re constantly asking when, we’ll never be able to finish our tasks so we can work on yours.

7. They Don’t Know Why You’re on This Medication
One thing you should know about are your meds and why you’re taking them. The nurse isn’t customarily in charge of explaining this to you.
Nurses are smart. We know hundreds of diseases and diagnoses, the medications that treat them, and how they work to treat each condition. However, many meds have multiple indications and various uses. For example, let’s say we know you have high blood-pressure (hypertension) and you’re scheduled to receive three meds. These three meds can be used for hypertension, but have very different mechanisms of action. We can find out why you’re taking them, but reviewing a patient’s history is kind of like reading a recorded version of the game “telephone.” Depending on who entered the information, who reviewed it, and assuming they haven’t missed anything important, we may safely infer that you have fairly resistant hypertension and that’s why you’re taking these meds, but it’s much better and easier if you take some responsibility for keeping track of what your doctors are prescribing and why.
On the other hand, clear communication is key when you’re in the hospital, and we know that sometimes you need to ask more than once to get things straight. Never be afraid to ask the question, “Why?” But then make sure you listen to and understand the answer!
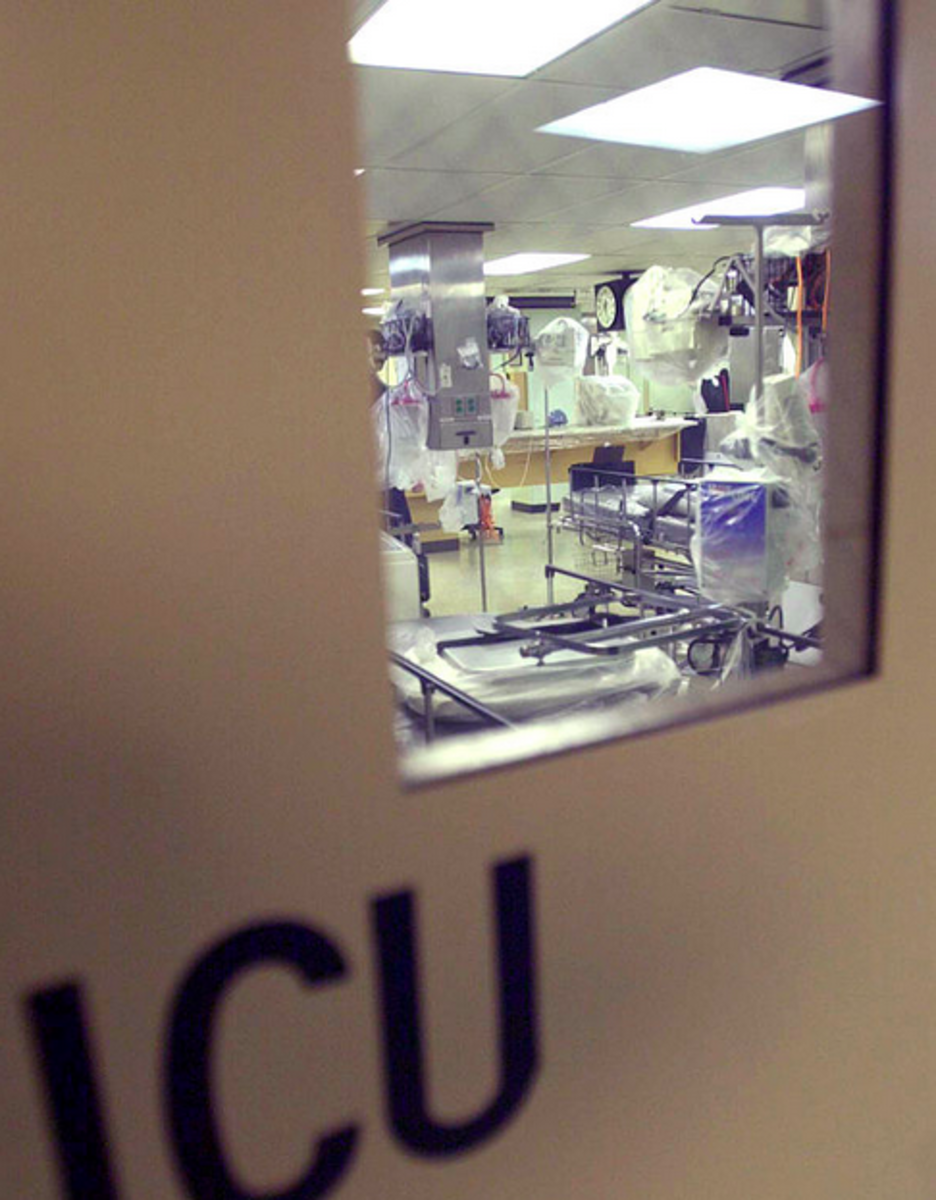
8. They Think You Should Be in the Intensive Care Unit
Nursing is an art and it takes experience to build skills like developing a gut reaction. Sometimes, you can just look at a patient and know that they should be in the intensive care unit. New nurses may not get it right away, but experienced nurses (as well as other medical staff) can sense an emergency from just a few feet away.
Many of us have various rituals to ward off these bad spirits, which may include plugging in the code cart just a little closer to your room or withholding lunch just a little bit longer to see how you’ll do. If your nurse or aide seems concerned about you (visiting you every ten minutes, constantly checking your vitals, and incessantly asks how you’re feeling), just tell the truth. Stoicism doesn’t work well in hospitals: not for pain relief, not for nausea, and especially not for “feeling the worst you’ve ever felt.”
If you feel that something is just not right, tell us. Sometimes our patients get that ominous feeling before we do, but all it takes is a little initiative to get us to take a longer look into your trending vitals, labs, and recent tests to determine if we need to call your provider to take a second look.

9. When You Say You’re Allergic to All Pain Meds Except Dilaudid…
We may roll our eyes. Just joking… okay, well, sort of.
“Pain is always what the patient says it is: Always.” However, if your pain is truly a 10/10, then joking, laughing, texting, and answering your phone when the nurse is asking you serious questions is not the best way to appear sincere.
Withholding pain medications for a person in pain is against the rights of the patient, and a nurses don’t withhold pain medications when a person is in pain, but be honest. Even a little pain is cause for intervention, but it’s not only the degree of pain you’re experiencing but the sincerity with which you express it that will get you the compassionate care you deserve.
10. Get Out of the Hospital as Soon as Possible
Hospitals are gross, period. We strive as hard as we can to sterilize, clean, and disinfect the thousands of germs that are harbored in the recesses of your hospital bed, remote control, bathroom, and floors, but it’s just not enough. And the longer you stay in the hospital, the greater risk you are of being infected with a nasty hospital super-bug.
Yes, there are horrible germs that cause everything from ventilator-associated pneumonia to MRSA and result in thousands of additional dollars in care. They may make you even more sick than you were in the first place. So if you’re fine but think one more day of rest in a nice hospital with friendly staff and prepared meals is a good idea, think again. Get out as fast as you can.

Thank You
That being said, you’re always welcome to visit when you’re well again. We always appreciate thanks from patients we’ve helped recover. You don’t need to bring cookies or treats, just a simple card or visit will do to remind us why we keep doing what we do. The smiles of previous patients make the long hours, stressful shifts, and overtime worth it. We didn’t choose this profession to be money-makers, but rather to provide honest and compassionate care so that you can return to a normal, happy, and healthy life.

